Vitamin D
A group of sterols involved in regulating calcium and phosphorus metabolism. Vitamin D2 (ergocalciferol) is found in plants. It is formed from provitamin ergosterol by the action of ultraviolet rays. Vitamin D3 is formed from provitamin 7-dehydrocholesterol in human and animal skin, under the influence of ultraviolet radiation during a non-enzymatic reaction. Only a small part of this vitamin is obtained from food (e.g., from animal fats, egg yolk, fish liver, sunflower, olive oil). Food calciferols are absorbed in the small intestine, with the participation of bile acids. They enter the lymph with chylomicrons, then into the blood and liver. Endogenous cholecalciferol also enters the liver with the blood. Neither vitamin D2 (ergocalciferol) nor vitamin D3 (cholecalciferol) are active. The most biologically active form of vitamin D is 1,25-dihydroxycholecalciferol – 1,25-(OH)2-D3 (calcitriol). Its structure and mechanism of action are similar to steroid hormones, so 1,25-(OH)2-D3 is called the D hormone.
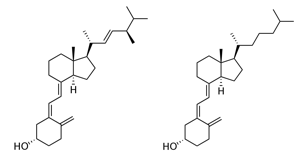
Vitamin D2 (ergocalciferol) Vitamin D3 (cholecalciferol)
1,25-dihydroxycholecalciferol is formed in two stages: in the liver and kidneys, catalyzed by enzymes hydroxylases (monooxygenases). Both hydroxylation reactions involve cytochrome P450, NADPH, Mg2+, and molecular oxygen. The formation of the active form of vitamin D is regulated by the hormone of the parathyroid glands – parathyroid hormone (PTH), as it stimulates the activity of 1-hydroxylase. In addition, the formation of 1,25-(OH)2D3 is regulated by a feedback principle. The active form of vitamin D – 1,25-dihydroxycholecalciferol (1,25-(OH)2D3), i.e., calcitriol, is regulated by parathyroid hormone and calcitonin from the thyroid gland, regulating calcium and phosphate homeostasis. The main importance lies with calcitriol and parathyroid hormone. Calcitriol regulates the absorption of calcium and phosphate ions in the small intestine, reabsorption in the kidney tubules, and bone mineralization. The main target cells of calcitriol are the cells of the small intestine, bone tissue, and kidney tubules. However, its receptors are also found in other cells: pancreas, brain, testes, uterus, placenta, mammary glands, etc. 1,25-(OH)2D3 binds to receptors (proteins) in the nuclei of target cells. The formed complex of calcitriol and the receptor in the nucleus activates genes encoding the synthesis of certain proteins. One of the most important functions of calcitriol is the transport of calcium and phosphate ions through the intestinal mucosa. In the intestinal mucosal cells, calcitriol induces the synthesis of proteins – calcium-binding protein (CaSB), Ca2+-ATPase, and others involved in transporting calcium and phosphate ions through the intestinal mucosa. Thus, 1,25-(OH)2D3 helps maintain a constant concentration of calcium ions and phosphate in the blood, which is necessary for bone formation and renewal. The effect of calcitriol on bones is twofold; anabolic and catabolic. It is necessary for proper bone mineralization. In bones, calcitriol promotes the synthesis of proteins that bind calcium – osteocalcin, osteonectin, etc. Additionally, calcitriol influences the growth and differentiation of bone cells. It acts on the precursors of osteoblasts and osteoclasts (stem cells) and accelerates the division of these immature bone cells into osteoblasts and osteoclasts. Calcitriol increases the number and activity of osteoclasts. Osteoclasts do not have receptors for calcitriol and do not react to vitamin D in isolation. Osteoblasts have calcitriol receptors and are target cells in bones.
Children who do not receive enough vitamin D from food or due to a lack of ultraviolet rays suffer from rickets (Gr. rachis – spine). In case of vitamin D deficiency, there is a disruption of calcium and phosphorus metabolism in the body: a decrease in Ca2+ and phosphate levels in the blood plasma, impaired mineralization of bone tissue, slowed bone growth. Bones become soft. Under the influence of body weight, they deform: the spine curves, leg bones take on an “X” or “O” shape. The ends of the ribs thicken instead of the bone-cartilage junction (rachitic rosaries), the chest protrudes forward (chicken breast), the head becomes large and deformed. Muscle hypotonia begins.
In adults, vitamin D deficiency leads to osteomalacia (softening of the bones). With a decrease in Ca2+ and phosphate absorption in the intestine, the renewal of bone tissue is disrupted, making the bones weaker. Vitamin D deficiency can occur in liver and especially kidney diseases, although an adequate amount is obtained from food: the formation of active vitamin D is disrupted, hypocalcemia begins, and kidney-origin osteodystrophy occurs. Vitamin D hypervitaminosis occurs if excessive doses are taken for a long time. Doses of vitamin D that are 10 times or more are toxic. Vitamin D hypervitaminosis is characterized by an increased concentration of calcium in the blood (hypercalcemia), calcification of various tissues, increased excretion of calcium in the urine (hypercalciuria). The increased calcium concentration in the blood is due to intensified calcium absorption in the intestine and demineralization of bones. Poorly soluble calcium salts deposit in internal organs – lungs, blood vessels, etc. Kidney stones can form in the kidneys. Vitamin D2 (ergocalciferol) is found in plant products: sunflower, olive oil, etc., while vitamin D3 (cholecalciferol) is found in animal food products: liver, fish oil, animal fats, less in butter, milk, cream. Vitamin D preparations are used for rickets prevention, tuberculosis of the bones, and treatment of certain skin diseases.
Source | Glossary of Most Commonly Used Biomedical Terms and Concepts | Lithuanian University of Health Sciences | Academician Professor Antanas Praškevičius, Professor Laima Ivanovienė
