Seasonal fluctuations in arterial blood pressure
Dr. Jūratė Barysienė1'3, Dr. Agnė Čerkauskaitė1'2, Prof. Dr. Marius Miglinas1'2
1 Vilnius University, Faculty of Medicine
2 VUH KF Nephrology Center
3 VUH KF Heart and Vascular Center
Impact of Cold on Cardiovascular and Cerebrovascular Diseases
Cold is one of the most important seasonal and circadian factors that increases the incidence and mortality from cardiovascular diseases and cerebrovascular diseases. Fluctuations in blood pressure depend on seasonal differences in ambient temperature. Low ambient temperatures increase blood pressure and mostly affect older individuals.
Increased sympathetic nervous system activity due to cold, season-dependent humoral changes, and vascular conditions lead to seasonal hypertension and its fluctuations.
To reduce mortality from cardiovascular and cerebrovascular diseases, experts recommend optimizing room temperature, changing lifestyle and behavior, and adjusting the doses and timing of antihypertensive medications according to the seasons.
Blood pressure changes related to low air temperature lead to higher mortality from cardiovascular diseases and cerebrovascular diseases: the risk of ischemic stroke in winter and spring is 20% higher than in summer, while the likelihood of acute myocardial infarction during the cold period increases by up to 53% [3, 4].
Clinical and epidemiological studies on healthy individuals of various ages, patients with hypertension (treated and untreated), dialysis patients, and transplant recipients have shown a relationship between seasons and blood pressure fluctuations [5].
Environmental Temperature and Seasonal Blood Pressure Fluctuations
Numerous studies have been conducted to evaluate the climate's impact on seasonal blood pressure fluctuations, and it has been found that outdoor temperature is the most important and independent factor influencing this phenomenon [6]. An increasing trend in both systolic blood pressure (SBP) and diastolic blood pressure (DBP) has been observed in winter [7]. Studies on large populations have shown that SBP differed by 4-9 mm Hg between summer and winter, while DBP differed by 0.6-5 mm Hg [8, 9].
Although seasonal temperature fluctuations affect individuals of all ages, older individuals are more affected. Studies conducted in the United States, the United Kingdom, Italy, Iraq, the Netherlands, Japan, Israel, and Russia show that seasonal blood pressure fluctuations differ significantly. These fluctuations are 18% higher in the older age group compared to younger participants with normal or elevated blood pressure.[7].
In the Three-City study, for individuals over 80 years old, the average SBP was 5 mm Hg higher in winter than in summer and was independent of anthropometric data and baseline blood pressure [10]. In the Medical Research Council treatment study involving 17,000 men, it was found that on cold winter days, the group aged 55-64 had a blood pressure 6-7/3-4 mm Hg higher, while the group aged 35-44 only had an increase of 2-4/2-3 mm Hg [11].
Climate Factors and Blood Pressure
S. Levington and colleagues analyzed the seasonal blood pressure fluctuations of half a million individuals aged 30-79 in ten different geographical regions of China with varying climate conditions. This was the first large-scale study that comprehensively assessed the relationship and impact of various factors (relative humidity, central heating, age, alcohol consumption, obesity, antihypertensive treatment, seasonal changes, and temperature fluctuations) on blood pressure fluctuations.
Data from a four-year observation showed that average blood pressure increased in winter compared to summer and that the difference in blood pressure between seasons was greater for rural residents than urban dwellers. In winter, older people and lean individuals (with a lower body mass index (BMI)) experienced higher blood pressure. Seasonal and temperature-related blood pressure fluctuations did not correlate with relative humidity or alcohol consumption.
In regions with warmer winters and moderate indoor heating, mortality was higher in winter, while in cold winter regions where more heating was used, mortality in winter was relatively lower [12]. Similar evidence was presented by K. Saeki and colleagues, who observed 147 Japanese residents. Blood pressure changes in rooms where the temperature differed by up to 10 degrees. Based on these results, the hypothesis was raised that optimal heating of rooms in winter could reduce blood pressure fluctuations and mortality [13].
Seasonal Daily Blood Pressure Fluctuations
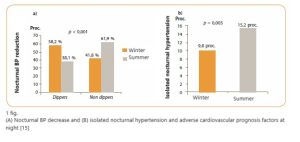
C. Thomas and colleagues, as well as G. Charach, state that the nature of circadian (i.e., daily) blood pressure fluctuations can change depending on the season [7, 14]. Different studies report varying numbers of blood pressure fluctuations. M. Fedecostante and colleagues, evaluating seasonal blood pressure fluctuations based on 24-hour blood pressure monitoring data in a group of patients living in a moderate climate zone (n = 1395, of which 89.3% had hypertension), identified how blood pressure changes depending on the time of day and described the relationship between seasonal variations and nighttime blood pressure as well as temperature and daytime blood pressure. In winter, systolic and diastolic daily blood pressure (p = 0.01) were higher, while in summer, nighttime systolic and pulse blood pressure were higher (2.3 mm Hg, p = 0.005; 1.0 mm Hg, p >0.05) [15].
The study revealed that higher air temperatures not only correlate with lower daytime blood pressure but also do not lead to a decrease in blood pressure at night. Among hypertensive patients, researchers observed a significant increase in nighttime systolic blood pressure during heatwaves, regardless of gender and age. They also noted the occurrence of isolated nocturnal hypertension (nighttime blood pressure: systolic >120 mm Hg or diastolic >70 mm Hg) (Figure 1).
It is still unclear what causes an increase in blood pressure at night during summer and why such blood pressure increases occur more frequently. Physical activity, quality and duration of sleep, environmental temperature, and differences in outdoor and indoor temperatures are all factors that can affect daily-nightly blood pressure fluctuations. However, it is believed that different sleeping habits and a reduction in medication doses during summer have the greatest impact on blood pressure differences [15].
Climate and Seasonal Effects on Blood Pressure
The effects of seasons on blood pressure can be short-term and long-term. Environmental temperature can quickly increase blood pressure (within 1-7 days) and gradually change with the seasons. Short-term temperature changes mostly affect daytime blood pressure, while seasonality mainly affects nighttime systolic blood pressure and morning blood pressure elevation.
The effects of short-term and long-term temperature changes on blood pressure often overlap, and other factors can also influence blood pressure. In a study by M. Morabito and colleagues found that during atmospheric changes (storms, wind, air masses transitioning from anticyclone to cyclone), daily blood pressure increased by 4 mm Hg (0 to 7 mm Hg) and nighttime blood pressure increased by 6 mm Hg (3 to 10 mm Hg) for several days. This increase occurred independently of BMI, age, gender, antihypertensive treatment (treated or untreated), number of antihypertensive medications, and daily weather changes such as temperature, cloud cover, relative humidity, atmospheric pressure, and wind [16].
Pathophysiological mechanisms of Neurohumoral regulation
Arterial blood pressure (ABP) depends on cardiac output, peripheral vascular resistance, and heart rate. In healthy individuals, cardiac output and stroke volume decrease by 10% and 15% in winter, respectively, while heart rate and peripheral vascular resistance increase by 5% and 11%, respectively (p <0.15) [7].
One of the most important roles in ABP regulation is played by the sympathetic nervous system (SNS). Cold activates the SNS and the renin-angiotensin-aldosterone system (RAAS). Increased release of norepinephrine, vasoconstrictive peptides (neuropeptide Y) causes arteriolar constriction and increases systemic peripheral vascular resistance, leading to an increase in heart rate and ABP [1]. In low temperatures, sweating and salt loss decrease, sodium concentration in plasma increases, and RAAS is activated [17].
An inverse relationship between daily urine volume and average environmental temperature in winter has been observed [13]. It has been proven that chilling the skin due to changes in vasomotor tone significantly increases peripheral vascular resistance and ABP. The increase in blood pressure also depends on vasoconstriction of internal organs such as the superior mesenteric and renal arteries during cold seasons [13]. According to the literature, the increase in plasma and urine epinephrine and norepinephrine levels related to cold occurs in both individuals with arterial hypertension and healthy individuals [17].
Vascular condition and ABP fluctuations
Arterial stiffness is an independent factor affecting seasonal ABP fluctuations [1, 18]. Pulse wave velocity (PWV), an indicator of vascular stiffness, correlates with winter-summer systolic ABP differences and depends on age [19]. In summer, peripheral vascular resistance decreases partly due to the suppression of baroreflex response caused by vasodilation of skin blood vessels [18].
Effect of Vitamin D on ABP fluctuations
It has been shown that daylight duration, i.e., the bright hours of the day, also affects ABP. Cold-induced vasoconstriction can affect blood components, lead to erythrocyte deformation, increase blood viscosity, peripheral vascular resistance, and ABP. Reduced levels of ultraviolet radiation in winter reduce the synthesis of vitamin D3 in the epidermis, therefore, due to vitamin D deficiency, the RAAS system is activated, and ABP increases [1].
Lifestyle and behavioral changes in different seasons
The onset or increase of hypertension in winter may also be influenced by increased consumption of salty foods, reduced physical activity, and weight gain [1]. Older people consume less fluids due to poor dietary habits and fear of urinary incontinence or heart failure, which also affects adaptive ABP factors in different seasons. Meanwhile, individuals who exercise regularly better tolerate cold-induced stress. Physiological adaptation mechanisms develop in them: humoral status changes (serotonin decreases) and vagal control increases; seasonal ABP fluctuations are lower in such individuals [13].
Other seasonal factors affecting ABP
According to clinical studies and observations, atmospheric pressure, rain, and climate humidity do not influence ABP. Lower stress in summer (during vacations), physical exercises, mood (bipolar disorder), cognitive function, behavioral changes, and biological processes are also important for ABP changes [7].
P. Siha et al., studying a female population in India, confirmed the associations between BMI and seasonal ABP fluctuations. The lower the body weight, the more significant the increase in ABP during winter compared to overweight, healthy, or obese individuals (p <0.05) [20].
Seasonal changes also affect laboratory test indicators.In winter, blood inflammation markers increase (e.g., CRP), and for people with diabetes, there is a significant increase in glycosylated hemoglobin, cholesterol, and fasting glucose concentrations [21, 22]. Activated factor VII coagulation, red blood cell and platelet counts also increase during the cold season.
These parameters can increase the risk of arterial thrombosis and cardio-cerebral diseases [1]. Y. Y. Al-Tamer et al. showed that the higher the ambient temperature, the lower the ABP and total cholesterol, and the higher the high-density lipoprotein cholesterol in healthy individuals and those with arterial hypertension (p <0.001) [23].
Treatment and recommendations
One of the most commonly used methods to assess sympathetic NS activity is the ABP response to cold. There is a known inverse relationship between diastolic ABP and room temperature [7], so ABP measurements in cold rooms can be misleading.
On the other hand, measuring ABP in a warm environment can also change ABP values. Therefore, guidelines for diagnosing and treating arterial hypertension recommend measuring ABP at a standardized room temperature.
Elevated blood pressure in winter or on cold days directly relates to an increased risk of cardiovascular diseases. With significant fluctuations in outdoor temperature, particularly in older people, careful monitoring of blood pressure is necessary.
Although antihypertensive medications do not protect against seasonal blood pressure fluctuations, antihypertensive treatment "softens" the response of the autonomic nervous system and autonomic tone to cold weather in winter, helping to better control blood pressure [24, 25].
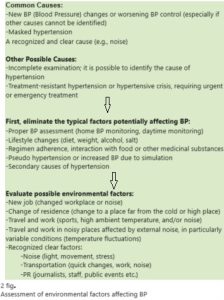
Treatment of Hypertension Considering Seasonal Blood Pressure Fluctuations In clinical practice, particularly with older people, the seasonal effect of temperature on blood pressure becomes evident. However, hypertension diagnostic and treatment guidelines do not categorize treatment by seasons, focusing instead on blood pressure control. Hypertension treatment should adjust according to the season. To distinguish seasonal blood pressure changes from other environmental factors influencing blood pressure differences, one can follow the algorithm proposed by R. D. Brook and colleagues.[25] (Figure 2). Antihypertensive Drug Classes Drugs such as metoprolol, carvedilol, lisinopril, eprosartan, amlodipine, compared to placebo, have little effect on cold-induced blood pressure elevation [26]. Drugs recommended for the treatment of arterial hypertension that act on the RAAS (especially angiotensin receptor blockers (ARB) and calcium channel blockers (CCB)) not only reduce blood pressure but can also provide additional protection against stroke [27]. Different classes of antihypertensive drugs affect blood pressure variability differently. When evaluating the impact of antihypertensive treatment on blood pressure fluctuations and clinical outcomes, treatment with calcium channel blockers and thiazide diuretics reduced blood pressure variability (by 19% and 13% respectively), while treatment with angiotensin-converting enzyme inhibitors (ACEI), ARB, or beta-blockers increased it by 8%, 16%, and 17% respectively (meta-analysis of 389 studies). Compared to placebo, blood pressure fluctuations are reduced the most in the CCB group (by 24%). Higher doses of CCBs reduce blood pressure variability, while increasing beta-blocker doses increase variability.Recommendations
Importance of Monitoring Seasonal Blood Pressure Fluctuations
Seasonal blood pressure fluctuations are clinically significant and can increase the risk of cardiovascular diseases. Due to these fluctuations, hypertension may go undiagnosed, untreated, or suboptimally treated. Monitoring blood pressure at different times of the year can help identify hypertension timely and initiate treatment.
Seasonal Monitoring and Management
As seasons change and temperatures fluctuate, especially in older patients, careful monitoring of blood pressure is advisable to prevent adverse effects. Patients with hypertension may need to increase medication doses or add medications in winter. Protection from low temperatures through better room heating, along with adjusting medication doses, can reduce blood pressure and mortality rates from cardiovascular diseases during winter.
Chronotherapeutic Approach
Experts recommend titrating antihypertensive treatment according to a "chronotherapeutic method adapted to seasonal needs." This ensures optimal blood pressure control both day and night throughout the year.
Summer Management
In summer, to avoid orthostatic hypotension during the hottest hours, controlling nighttime blood pressure is beneficial. Prescribing at least one antihypertensive medication at night can reduce the risk of cardiovascular diseases. If there is no symptomatic hypotension during this time of year, there is no need to reduce antihypertensive treatment.[1].
Source: "Lithuanian Doctor's Journal"