Tension headache. How to help a patient experiencing it?
Gabija Visockytė Vilnius University Faculty of Medicine
IntroductionRare is the person who can boast of never having experienced a headache - an annoying, exhausting, and often daily activity hindering sensation that occurs unexpectedly and can last from a few minutes to several days or even weeks. It is difficult to determine the exact prevalence of this symptom, but it is believed that more than 90% of people have felt a headache at least once in their lifetime, and approximately every other adult has had a headache at least once in the past year. Headache is the most common disorder of the nervous system worldwide (1). Headache is not a separate disease - it is just a symptom, a signal sent by the body that something is wrong. The causes of pain can be very diverse - from simple fatigue and stress to serious and dangerous diseases. For this reason, unusual, recurrent, strong, and prolonged headaches that are not relieved by medication should not be ignored and should prompt a visit to a doctor. There are many primary and secondary causes of headaches, so only a specialist who has performed all the necessary tests can make an accurate diagnosis and prescribe appropriate treatment.
Types of HeadachesAccording to the etiology, headaches are classified as primary (occurring without any other predisposing cause) and secondary (caused by underlying factors such as diseases, conditions, medications, or environmental factors). According to the Third International Classification of Headache Disorders from 2018, the following types of headaches are distinguished (2):
1. Primary headaches. a. Migraine - an episodic headache accompanied by various neurological, gastrointestinal, and autonomic nervous system disorders. It is estimated that more than 10% of people worldwide suffer from it. In 2010, migraine was identified as the third most common disease worldwide, and in 2015, it was declared the third most disabling disease among people under 50 years old. Migraines affect women twice as often - it is believed that inflammatory cytokines that activate certain hormonal mechanisms are more active in causing pain around nerves and blood vessels. b. Tension-type headache - the most common primary headache, occurring in 3% (lasting 15 days or more per month) and 70% (lasting less than 15 days per month) of the population. Often described as a pressing and tightening sensation, it may be related to stress or problems with the neck bones and muscle system. c. Trigeminal autonomic cephalalgias - episodes of intense unilateral pain occurring in the orbital, supraorbital, and/or temporal regions, lasting 15-180 minutes. This type also includes cluster headaches, which can occur in an acute episodic or chronic form. d. Other primary headache disorders. 2. Secondary headaches. a. Headache associated with head and/or neck trauma. b. Headache associated with head and/or neck vascular pathology. c. Headache associated with non-vascular intracranial pathology. d. Headache associated with the use or withdrawal of certain substances. e. Headache associated with infection. f. Headache associated with disturbances in homeostatic processes. g. Head or facial pain associated with skull, neck, eye, ear, nose, sinus, dental, oral, or other facial or neck structure pathology. h. Headache associated with a psychiatric disorder. i. Other headache disorders.
Tension-Type HeadacheTension-type headache is a disorder of the nervous system characterized by an increased tendency to weak and moderate intensity headache attacks (4). Despite numerous and comprehensive clinical studies, the pathophysiology of this pain is not entirely clear. It is believed that infrequent, episodic tension-type headaches are caused by increased stimulation of peripheral afferent neurons coming from the head and neck muscles. In the case of chronic illness, long-term muscle tension and psychological stress influence the development of pain, but these are not the only related factors. In some cases, patients may also have generalized increased pain sensitivity or a disturbance in the brain's pain perception centers.
Although this condition can be diagnosed in children, the highest incidence is found in the 40-49 age group. Tension-type headaches are more commonly diagnosed in women than men (ratio 5:4). This difference increases when it comes to the chronic type of the disease. There is a direct relationship between the level of education and the incidence of tension-type headaches (4, 5).
Clinical Symptoms
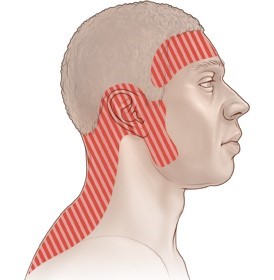
Easy episodic tension-type headache manifests as episodes of weak or moderate intensity headache, lasting shortly (rated ≤3 points on a visual analog scale), which resolve spontaneously or after taking common pain medications. Patients describe the pain as a sensation of muscle tightness, squeezing, or pulsating, felt symmetrically on both sides and sometimes described as a band around the head. Often the pain arises or may extend to the back of the neck (Figure 1). In this case, unlike in migraine, the headache rarely presents with additional symptoms such as sensitivity to light and sound, nausea, vomiting, loss of vision or speech, weakness of certain muscle groups, and others. The specific type of tension headache depends on the frequency of symptoms, their intensity, and response to common pain medications (5, 8).Rare episodic tension-type headache
Patients experience typical headaches lasting from a few minutes to several days. This type of pain does not worsen with regular physical activity and is not associated with nausea, although sometimes there may be a fear of light or sound. Diagnostic criteria: 1. At least 10 episodes of pain, occurring on average for 2. Pain lasting from 30 minutes to 7 days. 3. The pain presents with at least 2 of the following characteristics: a. Felt on both sides. b. Of pressing or tightening (non-pulsating) quality. c. Mild or moderate intensity. d. Not worsened by routine physical activity (e.g., walking or climbing stairs). 4. The pain features both of the following: a. No associated nausea or vomiting. b. Presents with no more than one of the symptoms: fear of light OR sound. 5. Does not meet the diagnostic criteria for other headache disorders.
Frequent episodic tension-type headacheAs the name suggests, this type of headache differs from the first type only in frequency of occurrence, with all other characteristics being the same. The key diagnostic criterion: 1. At least 10 headache episodes, occurring on average 1–14 days per month for more than 3 months (≥12 and Chronic tension-type headache This condition develops as a progression from frequent episodic tension-type headaches. Patients complain of very frequent (sometimes daily) usual-type headaches that can last from a few hours to several days or be constant. Diagnostic criteria: 1. Headache lasts on average for at least 15 days per year for more than 3 months (≥180 days per year) and meets 2–4 criteria. 2. Pain lasts from a few hours to several days or is constant. 3. The pain presents with at least 2 of the following characteristics: a. Felt on both sides. b. Of pressing or tightening (non-pulsating) quality. c. Mild or moderate intensity. d. Not worsened by routine physical activity (e.g., walking or climbing stairs). 4. The pain features both of the following: a. Presents with no more than 1 of the symptoms: fear of light OR sound OR mild nausea. b. No severe nausea and vomiting. 5. Does not meet the diagnostic criteria for other headache disorders.
Probable tension-type headacheA headache that does not meet any of the criteria for tension-type headaches but has characteristics typical of this type of pain. This diagnosis can only be made if no other headache disorder is identified in the patient (2, 3).
Diagnosis of tension-type headache The diagnosis of this condition is mainly based on collecting accurate patient medical and life history. To determine the type of headache affecting the individual, patients are often asked to keep a headache diary. In it, patients note: • When the pain starts (day and time). • How long the pain lasts. • The nature and intensity of the pain. • The locations where the pain starts and spreads. • Any additional symptoms that accompany the headache. • Circumstances when the pain began (it is important to pay attention to stress, lack of sleep, changes in eating habits, a woman's menstrual cycle phase, alcohol consumption, etc.). • What alleviates the pain. By analyzing the patient's diary entries for at least 1–3 months and considering the diagnostic criteria, it is possible to identify or at least suspect a specific type of tension headache. Laboratory or imaging tests are not useful for confirming the diagnosis and are not routinely performed. Additional patient evaluation may be recommended to rule out secondary causes of headaches if there is suspicion (6). Taking into account the characteristics of the patient's headaches and aiming to apply the most effective treatment, it is possible to perform differential diagnosis between different types of headaches (Table 1).Table 1. Differential diagnosis of different types of primary headaches (8, 9) + – characteristic feature, (+) – may be a characteristic feature, – – not a characteristic feature.
| Feature | Migraine | Tension-type headache | Cluster headache pain |
| Pain location |  |
 |
 |
| Photophobia | + | (+) | - |
| Phonophobia | + | (+) | - |
| Nausea and/or vomiting | + | - | - |
| Aura | (+) | - | - |
| Tearing | - | - | + |
| Rhinorrhea | - | - | + |
| Pain worsening under stress | + | - | - |
| Unilateral pain only | - | - | + |
| Positive response to triptans | + | - | + |
| Positive response to oxygen therapy | - | - | + |
Treatment of tension-type headache
The goals of treatment depend on the specific type of the condition. For episodic forms, symptomatic treatment is prescribed. Its main goal is to reduce pain and improve people's quality of life. If patients are adequate and cooperative, self-treatment with over-the-counter pain relievers may be recommended. In the absence of changes in headache symptoms (pain does not worsen, increase in frequency, or additional symptoms do not appear), long-term monitoring and care for these patients are not necessary. For very frequent episodic or chronic tension-type headaches, the primary goal of treatment is to achieve long-term remission of the condition. If this is not achieved, it is important to find a balance between symptom relief using pain medications and the risk of medication overuse, which can additionally cause secondary headaches and worsen the patient's overall condition. For this reason, patients complaining of chronic headaches are recommended to take only medications prescribed by a doctor, not increase their doses or frequency of use on their own, and periodically visit their family doctor.
Drug therapyFor most patients, effective symptomatic drug treatment for headaches can be prescribed if the episodes recur no more than 2 days a week. In this case, it is advisable to take over-the-counter pain relievers (aspirin 600–900 mg (except for children under 16 years old), ibuprofen 400 mg), sometimes it is indicated to use nonsteroidal anti-inflammatory drugs (ketoprofen 25–50 mg, naproxen 250–500 mg). Paracetamol (500–1,000 mg) is less effective (8, 10). Symptomatic treatment for chronic headaches is not possible due to the risk of medication overdose. These alternatives may be prescribed to these patients: • Naproxen 150–500 mg for a 3-week treatment course when the drugs are taken regularly every day. The goal of this treatment is to break the cycle of constant or frequently recurring headaches. If one treatment course was unsuccessful, it is not recommended to repeat it (10). • Amitriptyline - a drug from the class of tricyclic antidepressants, used in this case not for its properties related to reducing symptoms of depression. It has been found that starting treatment with small doses (10–25 mg at night) and increasing the dose every 1–2 weeks (by 10–25 mg) up to a final dose of 75–100 mg at night, the drugs act preventively and prevent the development of long-term or chronic headaches. If there is improvement after taking the drugs for 4–6 months, an attempt can be made to discontinue the treatment, hoping that the patient's health will not deteriorate. Treatment with tricyclic antidepressants may be unsuccessful due to too low a prescribed dose, insufficient treatment duration, or lack of patient cooperation - to avoid these obstacles, patients should be informed in advance about the type of drugs they will be treated with and what to expect during the treatment period (8, 10, 11).
If drug therapy is ineffectiveChronic tension-type headaches often can be resistant to drug treatment. For these patients, depending on their motivation and personal characteristics, it may be recommended to try nonspecific alternative treatment methods. Some pain clinics offer cognitive-behavioral therapy sessions, acupuncture of the neck and scalp muscles, and transcutaneous electrical nerve stimulation. These are not validated treatment methods, but for some patients, they alleviate the course of the disease, improve quality of life, especially when combined with amitriptyline drug therapy.
PreventionIt has been noticed that the development of tension-type headaches (especially episodic ones) is closely related to the influence of environmental factors. For this reason, in order to prevent headache attacks, patients are first recommended to change their lifestyle habits: • Tension-type headaches are more common in people with a sedentary lifestyle. Such patients are advised to include some form of physical activity in their daily routine - more walking or running outdoors, visiting a sports club, dancing, or engaging in another favorite sport. This not only improves physical well-being but also reduces stress. • Comprehensive physiotherapy may be recommended for people with bone and muscle system problems. Specialists, using massage, mobilization techniques, special exercises, and postural correction, reduce tension in the neck and shoulder muscles. This method is effective in treating a condition that developed after an injury. In the case of degenerative changes in the neck vertebrae, the results may not be as good. When starting physiotherapy, headache symptoms may initially worsen, but long-term improvement is achieved over time. • If patients indicate that headache attacks occur during or after stressful situations, various relaxation therapies may be recommended. During cognitive-behavioral therapy, patients can be taught various stress management methods, while others may find yoga or meditation more effective (8, 10, 11).
SummaryTension-type headaches - a common unpleasant sensation affecting many people, often worsening overall well-being, mood, and reducing productivity. By correcting lifestyle habits, the frequency of attacks can be minimized, and timely use of non-specific pain relievers ensures quick relief of symptoms. In rare cases, in the presence of a chronic form of the disease and aiming for disease remission, complex treatment with tricyclic antidepressants and non-drug measures may be necessary. It is important not to forget that drug overdose and the resulting secondary headache can further worsen the patient's condition.
Publication "Internistas" No. 8 2019.
Literature1. World Health Organization. Headache disorders, 2016. Available online: https://www.who.int/news-room/fact-sheets/detail/headache-disorders. 2. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018; 38(1), 1–211. 3. Benoliel R, Eliav E. Primary headache disorders. Dent Clin North Am. 2013 Jul;57(3):513-39. 4. Mier RW, Dhadwal S. Primary headaches. Dent Clin North Am. 2018 Oct;62(4):611-628. 5. Loder E, Rizzoli P. Tension-type headache. BMJ. 2008; 336 (7635): 88–92. 6. Chowdhury D. Tension type headache. Ann Indian Acad Neurol. 2012;15(Suppl 1):S83–S88. 7. Tension-Type Headache: Areas of Pain (illustration). Available online: https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=tp12150. 8. May A. Hints on Diagnosing and Treating Headache. Dtsch Arztebl Int. 2018;115(17):299–308. 9. American migraine foundation. Can Your Headaches Worsen in Number and Why? (illustration). Available online: https://americanmigrainefoundation.org/resource-library/can-your-headaches-worsen-in-number-and-why/. 10. British Association for the Study of Headache. National Headache Management System for Adults 2019. Available online: http://www.bash.org.uk/downloads/guidelines2019/01_BASHNationalHeadache_Management_SystemforAdults_2019_guideline_versi.pdf. 11. Bendtsen L, et al. EFNS. EFNS guideline on the treatment of tension-type headache - report of an EFNS task force. Eur J Neurol. 2010 Nov;17(11):1318-25.
